Medical billing is a complex and time-consuming task, especially with the risk of errors that can lead to legal trouble and rejected insurance claims. Fortunately, there is a solution: web-based medical billing software integrated within EMRs and EHRs. They help you make billing operations a breeze and provide remote access. But how do you choose the right one?
Compare Top Medical Billing Software Leaders
What This Article Covers
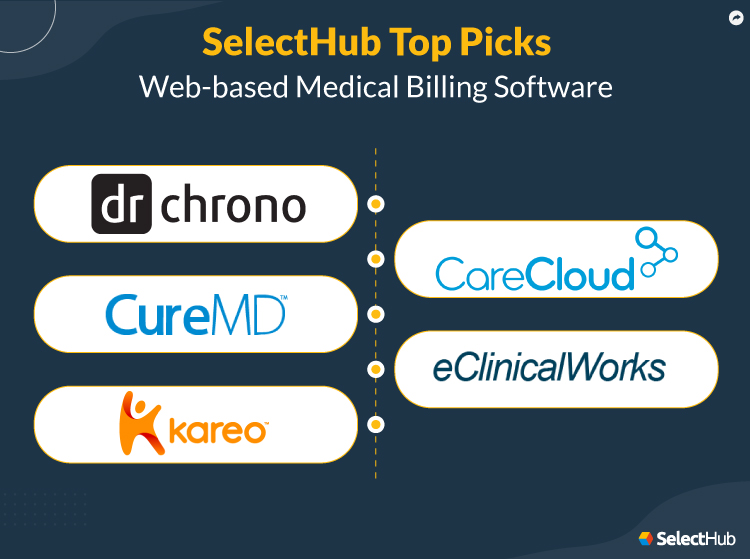
Best Web-based Medical Billing Software
Using a built-in algorithm based on market research, customer reviews and analyst input, our analysts rated each solution by category and determined an overall score.
DrChrono
DrChrono is a cloud-based EHR and practice management software that helps practices of all sizes streamline billing processes and manage patient data.
It offers features such as scheduling, claim management, insurance eligibility verification, payment processing and revenue cycle management. It also provides a patient portal and mobile app for secure communication and on-the-go access to patient data.
DrChrono offers pricing plans starting at $149 per month per provider. It also provides billing services for claim submission, revenue cycle management and denial management for an additional fee.
Create billing profiles with DrChrono to generate accurate bills. Source
Highest Rated Features According to Our Data
- Claims Management — 100
- Compliance and Security — 100
- Insurance Payments Management — 100
- Patient Payment Management — 100
- Pre-appointment Functionalities — 100
Top Benefits
- Maximize Revenue Collection: Revenue cycle management modules enable you to automate tasks such as claims submission and payment posting to help you get paid faster and improve cash flow.
- Reduce Denials: Create customized billing rules, such as specific codes for certain procedures, to help produce accurate bills. Claim scrubbing functionality enables you to identify errors to aid you in producing clean claims.
- Boost Productivity: Built-in templates, speech-to-text and photo-charting functionalities help reduce administrative burdens. Integrate with patient scheduling tools and patient engagement products to streamline workflows and deliver value-based care.
- Make Data-driven Decisions: Reporting modules allow you to track key performance metrics such as A/R days and denial rates to help you improve your billing processes.
- Ensure Data Security: Store sensitive data securely and meet meaningful use standards. SSL/TLS encryption capabilities help you secure data transmission between devices and servers.
Primary Features
- Billing Profiles: Set ICD-10, CPT/HCPCS and NDC codes to the most common procedures to reduce data entry errors and save time. You can generate accurate bills with just a few clicks.
- Eligibility Verification: Check insurance eligibility before appointments in real time to reduce denials.
- Patient Statements: Attach notes, charts and due dates to statements. Preview and send statements to patients from within the system to save time.
- Claims Management: Submit claims electronically to save time. You can utilize clearinghouse connections like TriZetto, Waystar, Change Healthcare, Jopari and Carisk Partners to reduce coding errors and prevent rejections. Process multiple claims simultaneously with an option to manage write-offs through the adjustment’s master screen on the solution’s dashboard.
- BI Tools: Generate and analyze reports using BI tools to monitor your practice’s performance and optimize billing operations. Obtain snapshots of incoming payments through the payment analysis tool. Spot root causes of denials using the denial analysis modules.
Limitations
- Steep learning curve.
- Frequent system crashes.
- Unresponsive customer support.
Features Not Fully Supported According to Our Data
- Automated Report Scheduling — Not Supported
- Natural Language Diagnosis Codes Search — Supported With Partner Integrations
- Barcode Scanner Software Integration — Not Supported
- Prior Authorizations — Supported With Partner Integrations
- Offline Access — Not Supported
Platform:
Company Size Suitability: S M L
CureMD
CureMD helps health care providers streamline billing operations, improve revenue capture, deliver quality patient care and increase cash flow.
It provides payer management, electronic claims tracking and submission, electronic remittances, automatic charge capture, clean claim checks, and electronic payment posting modules.
It offers flexible pricing options, enabling you to choose a plan according to your needs. To get a quote, you can contact CureMD’s sales team.
The vendor provides a team of experienced professionals who’re trained to handle all aspects of medical billing and revenue cycle management. Plus, the option for specialty medical billing modules like Neurology medical billing, Cardiology medical billing, and Obgyn medical billing among others is also a good feature.
Monitor financial metrics like charges and payments with CureMD. Source
Highest Rated Features According to Our Data
- Claims Management — 100
- Insurance Payments Management — 100
- Patient Payments Management — 100
- Point of Care Functionalities — 100
- Pre-appointment Functionalities — 100
Top Benefits
- Increase Reimbursements: Stay ahead of compliance requirements and accelerate collections using medial practice management tools. Submit claims electronically to save time and receive payments quicker.
- Improve Productivity: Access patient data from remote locations using the Avalon EHR app. Dictate via Siri to speed up note-taking and focus on crucial tasks.
- Reduce Claim Rejections: Detect coding mistakes using claim scrubbing functionality. The system comes with over 2,500 policy formats, ensuring you submit claims correctly the first time.
- Deliver Quality Patient Care: View clinical summaries in the continuity of care format and create treatment plans within minutes. Patients can enter demographic details online based on predetermined parameters. They can also book online appointments, make electronic payments and securely communicate with providers via the patient portal tool.
- Achieve Interoperability: It enables you to integrate with third-party EHRs, allowing for seamless communication and documentation between the two systems which in turn helps you generate accurate statements.
Primary Features
- Eligibility Verification: You can verify patients’ insurance eligibility within minutes to help reduce administrative burdens.
- Claim Scrubber: Detect coding errors and achieve a clean claims rate. Crosscheck national drug codes to improve reimbursement processes.
- Claim and Denial Management: Generate and submit claims to insurance companies either through electronic data interchange (EDI) or by mail in CMS-1500 format. Automatically identify and track denied claims to resolve issues on time. The built-in rules engine helps you manage denials effectively.
- Point of Sale: Create payment plans to improve patients’ financial experiences. Accept payments from clients through integrated credit card processing functionality.
- Financial Reporting: You can produce A/R aging, outstanding balance, collection ratio and service reports to forecast trends and make data-driven decisions.
Limitations
- Isn’t compatible with mobile devices.
- Doesn’t offer handwriting recognition functionality.
- Doesn’t provide a customized workflow for dental specialties.
Features Not Fully Supported According to Our Data
- FIPS 140-2 Compliance — Not Supported
- Automated Report Scheduling — Not Supported
- Natural Language Diagnosis Codes Search — Not Supported
- Speech-to-Text Dictation — Not Supported
- Insurance Card Scanning Software Integration — Not Supported
Platform:
Company Size Suitability: S M L
Kareo Billing
Kareo Billing helps small to medium-sized health care practices optimize billing processes, automate coding tasks and generate precise patient statements, improving revenue collections.
It provides automated claim submission, claims tracking, payment posting, denial resolution, insurance eligibility verification and reporting functionalities.
Its standard billing essential pricing plan costs $374 per month per provider, whereas the low volume pricing option costs $199 per month per provider. The vendor charges extra for add-ons.
The provider offers a team of billing experts to help you identify revenue opportunities and collect faster. They also provide a mailing service to accelerate collections.
Kareo Billing’s analytics function. Source
Highest Rated Features According to Our Data
- Claims Management — 100
- Insurance Payments Management — 100
- Patient Payments Management — 100
- Point of Care Functionalities — 100
- Pre-appointment Functionalities — 100
Top Benefits
- Go Paperless: Electronic charting, billing, scheduling and reporting capabilities help you accelerate operations and reduce the need for paper documents and administrative supplies.
- Simplify Workflows: Automated functions enable you to avoid repetitive tasks and reduce data entry mistakes.
- Reduce Coding Errors: The claim scrubber enables you to follow the coding rules published by the National Correct Coding Initiative (NCCI/CCI), Centers for Medicare and Medicaid Services (CMS) and American Medical Association (AMA).
- Improve Revenue Collection: Run insurance eligibility checks to avoid revenue leakage. Claim management modules help you reduce denials and improve reimbursement rates. Enable clients to make payments by scanning QR codes.
- Build a Profitable Business: Observe trends, identify revenue opportunities and generate financial reports to make strategic decisions. Group denials by reason to streamline the appeals process to help address similar denials together with a unified response.
Primary Features
- Billing Dashboard: Access medical records, track tasks and payments, schedule appointments, store documents, and generate reports from a single screen.
- Payment Posting: You can post insurance payments electronically to improve productivity and save time. Save and export electronic remittance advice reports to speed up payment processes.
- Insurance Enrollment: Submit transfer-of-authorization forms to allow the vendor to simplify enrollment processes. Use the search box to find insurances. Access the electronic enrollment dashboard to stay updated about claim statuses.
- Charge Capture and Patient Statements: The calendar view allows you to capture charges quickly. Track encounters, set up fee schedules and check codes through the encounter review window. Send electronic statements to patients for faster payments.
- Claims Management: Send electronic claims to more than 8,000 commercial companies and government payers. Generate validation reports to identify claims with missing patient information and incorrect policy and group numbers.
Limitations
- Limited reporting functionalities.
- Steep learning curve.
- Potential glitches while using the online payment platform.
Features Not Fully Supported According to Our Data
- Authentication — Not Supported
- HL7 Standards — Not Supported
- Native Mobile Applications — Moderately Supported Out of the Box
- Offline Access — Not Supported
- Calendar Support — Not Supported
Platform:
Company Size Suitability: S M L
CareCloud
CareCloud is a cloud-based solution designed for medical practices of all sizes. It assists you in automating workflows, saving time and money.
It provides patient engagement, telemedicine tools, credentialing, denial resolution, reporting and claim management modules to help you optimize your revenue cycle.
You need to contact CareCloud’s sales team to uncover pricing options.
The vendor offers a team of billing experts to help you reduce administrative burdens. They also help you send statements to patients on your behalf. Account managers assist you in keeping your practice compliant.
CareCloud’s account receivable dashboard. Source
Highest Rated Features According to Our Data
- Dashboards and Reports — 100
- Insurance Payments Management — 100
- Patient Payments Management — 100
- Alerts and Notifications — 100
- Pre-appointment Functionalities — 100
Top Benefits
- Increase Operational Efficiency: Automate tasks using practice management modules to streamline workflows. Schedule appointments using drag-and-drop functionality.
- Reduce Coding Errors: Take advantage of automated billing rules to avoid costly mistakes.
- Prevent Claim Denials: The vendor offers a clinical coding knowledge base to help you submit accurate claims and improve collections.
- Make Informed Decisions: Generate and analyze financial reports to optimize your practice for better financial outcomes.
- Ensure Data Security: Store patient information on a secure cloud-based server.
Primary Features
- Credentialing: Help your staff maintain their credentials with government and commercial payers to stay out of legal troubles. The vendor also offers Council for Affordable Quality Care (CAQH) quarterly re-attestations.
- Insurance Verification: Check patients’ insurance details like deductibles or copayments within a few minutes to reduce denials. You can also schedule overnight batch checks to focus on other important work and save time.
- Claim Management: Automatically identify and fix claim errors using claim scrubbing functionality. Submit claims digitally in just a few clicks to improve collections.
- Patient Billing: Streamline coding processes and capture charges while preventing costly mistakes. Billing rules enable you to generate accurate claims.
- Analytics: Observe trends to help discover areas needing improvement. Create a scorecard to keep track of your practice’s performance. Filter metrics by providers, locations and more to strategically alter workflows.
Limitations
- Isn’t compatible with Android devices.
- Doesn’t offer drill-down reporting.
- Doesn’t provide seamless navigation.
Features Not Fully Supported According to Our Data
- Claims History — Supported With Partner Integrations
- FIPS 140-2 Compliance — Not Supported
- Natural Language Diagnosis Codes Search — Not Supported
- Offline Access — Not Supported
- Charge Capture — Supported With Partner Integrations
Platform:
Company Size Suitability: S M L
eClinicalWorks
eClinicalWorks is a comprehensive electronic health record solution that caters to single and multi-specialty practices.
It provides patient scheduling, reporting, claim scrubbing, billing, payment processing and revenue management modules. The revenue cycle management console helps billing companies filter claims and communicate with practices effectively.
Its pricing plan (EHR with practice management) costs $599 per month per provider. You can contact the provider to uncover customization costs.
A billing team assists you in maximizing reimbursements with clearinghouse integration, a rules engine and canned reports packages.
eClinicalWorks security and compliance dashboard. Source
Highest Rated Features According to Our Data
- Claims Management — 100
- Medical Coding — 100
- Patient Payments Management — 100
- Automated Billing System — 100
- Point of Care Functionalities — 95
Top Benefits
- Ensure Interoperability: Its proprietary Health Information Exchange (HIE) platform allows you to share patient data across different health systems, ensuring continuity of care. It also supports various data exchange protocols such as HL7 FHIR and CCD.
- Improve Collections: Generate and send self-pay electronic statements to mailing services. The rules engine helps you speed up claims processing operations.
- Optimize Payment Workflows: Clients can make online payments via the patient portal, kiosk, mobile devices, and debit or credit cards.
- Deliver Quality Patient Care: Spend less time documenting patient data using EHR tools. The vendor offers patient management services to help identify and resolve existing client engagement issues.
- Stay Mobile: Store and access data from anywhere, at any time via the Google Chrome browser or iOS devices. The Healow app enables you to conduct meetings from remote locations. You can also send pre-visit forms and monitor vitals within minutes.
Primary Features
- Revenue Cycle Management: Use the patient cost estimator to view performed procedures and prepare an estimated cost plan. Patient payment integration enables you to process credit cards and ACH transactions to help increase collections.
- Electronic Health Records: Pull up patient records from primary care providers, clinics, care centers and hospitals via the PRISMA health information search engine. Exchange data with Cerner and EpicCare systems via the CommonWell Health Alliance and Carequality framework to make better clinical decisions.
- Patient Engagement: Patients can complete check-ins, answer questionnaires and confirm insurance information through kiosks. Create patient satisfaction surveys to provide quality care.
- Eligibility Verification: Check patient eligibility and benefits in real time to verify patient coverage, reduce the risk of claim denials and speed up the reimbursement process.
- Population Health Management: The health care effectiveness data and information set enables you to assess patients’ needs. Identify coding gaps using the hierarchical condition category module. Compare risk adjustment factor scores and analyze trends via the hierarchical condition category dashboard.
Limitations
- Occasional crashes.
- Difficult integration implementation.
- Complex navigation.
Features Not Fully Supported According to Our Data
- FIPS 140-2 Compliance — Not Supported
- Automated Report Scheduling — Not Supported
- Prior Authorizations — Supported With Partner Integrations
- Mobile Push Notifications — Not Supported
- Offline Access — Not Supported
Platform:
Company Size Suitability: S M L
Benefits and Drawbacks
Several industries, including health care, use software to optimize business operations. And the demand for online medical billing software continues to grow.
According to a report published by MarketsandMarkets, the global cloud computing market is projected to reach $1.2 trillion by 2027, growing at a CAGR of 17.9%.
Understanding both the benefits and limitations of web-based medical billing solutions is crucial in determining whether or not it’s the right solution for your practice. We’ve listed the same below to help you make informed decisions.
Some benefits of online medical billing systems include:
- Speed Up Processes: Manually reminding clients about appointments, payments and refill requests is daunting. With online software, you can set auto-reminders to enhance patient experiences and save time.
- Increase Collections: According to PYMNTS’ Digital Platform Promise report, 25.4% of consumers prefer paying medical bills through digital portals. Billing products enable patients to make electronic payments, helping you maximize profits.
- Improve Accuracy: We can’t memorize medical codes. And incorrect coding can lead to billing errors. Web-based billing software helps you translate notes into codes using natural language processing.
- Stay Mobile: You can access data from the comfort of your home by logging in to the product’s website. You can share data across your practice, enhancing collaboration between employees.
- Save on Costs: Typically, cloud-based products cost less compared to on-premise solutions upfront. Investing in SaaS applications also helps you cut down on IT expenses.
Don’t forget to create an implementation plan. It’ll help you identify potential issues and prevent project delays.
Some potential drawbacks of cloud-based medical billing solutions include:
- Extended Fees: Cloud-based software typically requires a subscription fee, which can add up over time. You might even have to pay extra for technical assistance and upgrades.
- Limited Device Integrations: Not all web-based products integrate with external devices like MRIs and ultrasounds. Some application service providers (ASPs) host the software on their servers and provide remote access to it via the internet to help you extract data from external machines.
- Unexpected Vendor Downtime: If the software provider experiences downtime or technical issues, you’ll be unable to perform medical billing tasks in a timely manner.
- Reduced Offline Access: As web-based software requires an internet connection, any loss of connectivity can cause delays.
Types of Buyers
Do you need an invoicing system that integrates with your EHR, or do you need something to help you manage clients claims? We’ve categorized these needs in the table below to make it easier for you to select a perfect product.
| Buyer Type | Buyer Needs | Required Modules |
|---|---|---|
| Integrated Suite Buyers | Practice management | Scheduling, billing, RCM, EMR and PACS |
| Inpatient Care Providers | Submitting claims using UB-04 forms | Claim submission and inpatient billing |
| Outpatient Care Providers | Submitting electronic claims using CMS-1500 forms | Claim management and Invoicing |
| Specialists | Receiving payments through cash, check or credit card | Online payment portal |
| Outsourced Services | Submitting claims on behalf of clinics or hospitals | Claim management, denial resolution, payment processing and charge capture |
Note: The table above highlights only essential modules needed according to the buyer type. You might also need other functionalities to achieve operational efficiency and deliver quality patient care. Remember to assess your needs before making a decision.
Market Trends
Mobile Computing
Because mobile applications provide remote capabilities, there’s a gradual increase of the adoption of mHealth products among health care providers.
According to a report published by Grand View Research, the global mHealth market is anticipated to grow at a CAGR of 10.8% from 2023-2030.
Mobile computing helps you:
- Capture patient information and update medical records.
- Simplify collection processes.
- Track and analyze billing data.
If you want to perform billing tasks on the go, consider medical billing software that provides robust mobile capabilities.
ONC-ATCB Certification
The U.S. government offers CMS and non-CMS incentives if you use ONC-ATCB certified EHRs, so always check with vendors about their certification.
You can check a product’s certification status via the Certified HealthIT Product List to make informed buying decisions.
Artificial Intelligence
AI-powered tools enable you to automate repetitive and time-consuming tasks. They can identify incorrect coding and suggest corrections to help you generate accurate bills and comply with health care regulations.
They also allow you to analyze large volumes of data to identify patterns and trends to assist you in maximizing revenue and reducing denials.
FAQs
What is a web-based medical billing solution?
Web-based medical billing software is a medical solution that helps you streamline medical billing processes, avoid coding errors and improve your practice’s financial performance. They offer A/R management, denial resolution, claim submission, reporting, payment posting and eligibility verification modules.
How will a web-based solution improve my business processes?
With a web-based solution, you can access data from anywhere, anytime. You can generate financial reports to make strategic decisions and increase revenue collections. Furthermore, you can customize your workflows and take advantage of automated functionalities.
Are web-based medical billing applications compliant with health care regulations?
Most online medical billing software comply with regulations such as HIPAA and the HITECH Act. You should select a vendor that regularly monitors and updates the system to maintain security and compliance.
In addition, look for an app that offers features such as data encryption, access controls and audit trails to ensure confidentiality and data integrity.
How do I select a web-based medical billing system?
To begin, you can conduct surveys to gain insights into your organization’s needs. Evaluate your and your staff’s needs to create a medical billing software features and requirements checklist.
Then, create a scorecard to determine which vendor best suits your necessities.
Finally, decide which product can enhance your workflow and drive your practice to success.
Note: Billing needs for practices and companies differ in terms of scale and complexity. If you run a billing service, you might require medical billing services solutions that provide additional workflow tools, code scrubbing, performance reporting and appeal managing capabilities.
Next Steps
Many health care technology trends have emerged over recent years. These innovations have had a profound impact on the functioning of medical industries. They help practitioners automate and speed up processes.
Most medical billing software programs provide similar features. So how do you select one that best suits your needs? You can use our comparison report to make informed buying decisions.
What’re your thoughts on the best web-based medical billing software? Have you had any experiences with the platforms mentioned in this article or any others? Share your thoughts in the comments below. We’d love to hear your insights and recommendations!
Analyst-Picked Related Content
Pricing Guide: Discover the true cost of Medical Billing software
Comparison Report: An Interactive analyst report with comparison ratings, reviews and pricing